

Greetings
Palliative care is a type of medical care that begins in the early stages of a cancer diagnosis. At our hospital, a multidisciplinary team of doctors, nurses, pharmacists, nutritionists, and other professionals will work with patients based on their circumstances. We strive to provide safe and reliable medical care that alleviates holistic suffering, so please feel free to consult with us. It is essential to provide seamless medical care by forming a network that brings together hospitals, clinics, private practice doctors, and home care doctors. We would like to work to build a network with all medical professionals.
Head of Palliative Care
Makoto Tokuhara
Treatment details and target diseases
Palliative care is not care provided after cancer treatment has ended, but instead begins early at the time of cancer diagnosis and is provided in parallel with treatment. Furthermore, the World Health Organization (WHO) has expanded palliative care beyond cancer to include HIV, incurable neurological diseases, chronic heart failure, chronic obstructive pulmonary disease (COPD), dementia, and liver failure, a future challenge. Cancer pain is holistic, consisting of physical, mental, social, and spiritual pain, and alleviating this pain is essential to improving patients' quality of life. Our multidisciplinary staff, including doctors, nurses, pharmacists, nutritionists, occupational therapists, and social workers, is involved in palliative care, working to alleviate symptoms and improve the quality of life for patients with physical and mental symptoms and their families.
As an acute care hospital treating many surgically eligible patients, we need to build close relationships and cooperate with all related medical facilities to ensure continuity of medical care. Furthermore, depending on the patient's condition, there are cases where the patient would be more satisfied if they spent their time at a hospital with a palliative care ward or a hospice rather than at an acute care hospital like ours. In such cases, we work closely with the patient's primary care physician and the Medical Collaboration Center after sufficient discussion to provide better medical care and nursing. Furthermore, we actively collaborate with the patient's primary care physician both within and outside our hospital, implementing joint medical treatments, introducing palliative care early, and maintaining cooperation to provide palliative care even after discharge.
Physical care
Pain is one of the most common physical sufferings experienced by cancer patients. It is said that approximately 80% of cancer patients experience some form of pain. Still, much of this pain can be controlled through the appropriate use of analgesics in combination with radiation therapy and nerve blocks. Cancer-related symptoms, in addition to pain, include fatigue, loss of appetite, cachexia, nausea, vomiting, constipation, ascites, dyspnea, and insomnia. A multidisciplinary team works to alleviate these symptoms through a combination of various drug therapies and non-drug care. However, as these symptoms become more severe, they severely limit patients' daily lives and can even undermine their human dignity. Therefore, it is essential to pay attention to their mental health. To that end, from the time of cancer diagnosis, we work with patients to alleviate their mental anguish in addition to alleviating their physical symptoms, striving to ensure their comfort.
Mental care
Many cancer patients experience a variety of emotional reactions as they are informed of their illness, and as their condition and treatment methods change. They may feel at a loss due to fear and anxiety, or experience anxiety-inducing treatment situations, sudden changes in mood and mental functioning during treatment, and even physical symptoms due to mental distress. We strive to alleviate the various types of pain experienced by such patients.
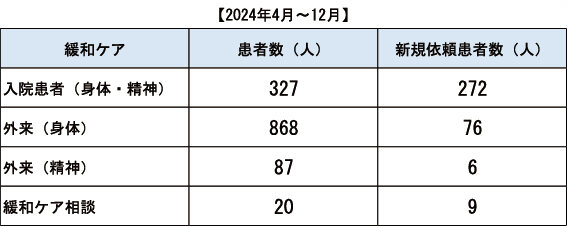
Main medical achievements
We respond to requests for pain relief for various cancer patients, but we tend to receive more requests from patients in the ENT and gynecological fields.
About Palliative Care Training Seminars
Department of Palliative Care provides palliative care to patients and their families who are undergoing cancer treatment at our hospital or nearby medical institutions. This care covers a wide range of periods, from immediately after a cancer diagnosis to the end of life. The department is run by a total of 11 staff members: two doctors specializing in physical symptoms, one doctor specializing in psychiatric symptoms, three doctors with other roles, two full-time nurses, one part-time pharmacist, and two part-time nutritionists.
In-hospital medical care works in cooperation with other departments involved in cancer treatment, striving to alleviate the physical and mental pain caused by drug therapy so that cancer patients and their families can receive cancer treatment without pain. Last year, we were involved in palliative care for approximately 300 cases, ranging from the five primary cancers, as well as rare skin cancers and adult malignant tumors such as brain tumors, to pediatric cancer. In addition to alleviating this physical and mental pain, we also work with nurses in the General Consulting Office, which certified social workers staff, and the home medical care room to address social anxiety associated with cancer treatment and to make home cancer treatment after discharge as painless as possible. We also provide information and education on in-hospital palliative care, as well as consultation and guidance on cancer-related lymphedema.
In addition, our hospital hosts palliative care training sessions twice a year to ensure that all medical professionals involved in cancer treatment acquire basic knowledge about palliative care. In addition to these training sessions, we also host study sessions for medical professionals involved in palliative care in the region and hold joint conferences to promote medical cooperation with the local community.
List of Palliative Care Training Seminar Graduates
Those who have completed training based on the "Guidelines for Holding Palliative Care Training Seminars for Physicians Involved in Cancer Treatment" (Notification No. 0401016 from the Director-General of the Health Bureau of the Ministry of Health, Labor and Welfare, dated April 1, 2008)
As of April 1, 2023
Doctor List
Department Head: Makoto Tokuhara
Outpatient: 0463 (93) 1121 extension 6351
Specially Appointed Professor Makoto Tokuhara
| Specialization | Palliative care |
|---|---|
| Specialist | Certified physician and specialist of the Japanese Society of Palliative Medicine, accredited physician of the Japanese Surgical Society, certified cancer treatment physician, specialist, and instructor of the Japanese Society of Gastroenterology |
| Specialized Areas | Palliative care (physical symptoms), pain management |
| Outpatient medical day | Monday, Tuesday, Wednesday, Friday (PM) |
Associate Professor Banri Tsuda
| Specialization | Palliative care, medical oncology |
|---|---|
| Specialist | Specialist and instructor of the Japan Surgical Society / Specialist and instructor of cancer chemotherapy at the Japanese Society of Clinical Oncology / Breast specialist and instructor at the Japan Breast Cancer Society / Certified cancer treatment physician / Certified industrial physician / Medical education specialist / Specialist of the Japanese Society for Palliative Medicine |
| Specialized Areas | Palliative care (physical symptoms), cancer immunotherapy |
| Outpatient medical day | Monday, Thursday, Friday (PM), Wednesday (AM, PM) |
Lecturer: Yuki Takahashi
| Specialization | Clinical Psychiatric Palliative Care |
|---|---|
| Specialist | Specialist and instructor of the Japanese Society of Psychiatry and Neurology |
| Specialized Areas | Pharmacotherapy and psychotherapy for general mental illnesses, diagnosis and treatment of cognitive symptoms associated with physical ailments, palliative care for mental symptoms in cancer patients, support for rehabilitation into society, and support for families |
| Outpatient medical day | Thursday (PM) |
Lecturer: Hiromi Tomomatsu
| Specialization | Palliative care, respiratory diseases |
|---|---|
| Specialist | Certified physician and specialist of the Japanese Society of Palliative Medicine / Certified physician for cancer treatment in Japan / Certified internist and specialist in General Internal Medicine by the Japanese Society of Internal Medicine / Japanese respiratory specialist and specialist / Japanese Society of Allergology |
| Specialized Areas | Palliative care (physical symptoms), pain management |
| Outpatient medical day | Mondays and Wednesdays (PM) |
Miho Ito (Part-time doctor)
| Specialization | anesthesia |
|---|---|
| Specialist | Japanese Society Department of Anesthesiology Supervisor / Japanese Society of Pain Clinicians Specialist / Japanese Society of Palliative Medicine Certified Doctor |
| Specialized Areas | Pediatric anesthesia, pain management, and palliative care |
| Outpatient medical day | Tuesday (PM) |
Harumi Saito (Part-time doctor)
| Specialization | Grief care |
|---|---|
| Specialist | Clinical Spiritual Care Practitioner of the Japan Society for Spiritual Care/Certified Clinical Listener of the Grief Care Research Institute of Sophia University |
| Specialized Areas | Grief care |
| Outpatient medical day | Tuesday (PM) |


